Rare Disorder Research Yields Insights into Immune Dysregulation, Drug Approaches
 July 7, 2023 – By studying a rare immune disorder, researchers in Seattle Children’s Research Institute’s Center for Immunity and Immunotherapies (CIIT) and colleagues have identified a new driver of autoimmunity that may be relevant to many other diseases, including lupus. Their findings were recently published in Science Translational Medicine.
July 7, 2023 – By studying a rare immune disorder, researchers in Seattle Children’s Research Institute’s Center for Immunity and Immunotherapies (CIIT) and colleagues have identified a new driver of autoimmunity that may be relevant to many other diseases, including lupus. Their findings were recently published in Science Translational Medicine.
The researchers studied the immune systems of children with STAT1 gain-of-function (STAT1 GOF) syndrome, a rare disease characterized by persistent Candida fungal infections; other viral, bacterial and fungal diseases; and a predisposition to autoimmune disorders, such as lupus and Type 1 diabetes. STAT1 GOF patients carry activating (“gain-of-function”) genetic mutations in a protein called STAT1 which regulates several important immune-signaling pathways implicated in human disease. By comparing the immune systems of healthy children and those with STAT1 GOF, this comparative work provided insights into how changes in STAT1 can cause a child’s immune system to become dysregulated and develop autoimmune disorders.
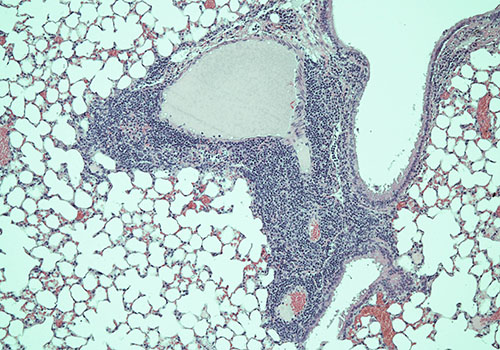
Since STAT1 GOF syndrome is a rare disease with limited human samples available, the researchers also developed a new mouse model of the disease. This strain developed immune system dysregulation similar to humans with the same STAT1 mutation, which allowed the research team to better understand the immune mechanisms causing STAT1 GOF syndrome. For example, despite clinical similarities between STAT1 GOF syndrome and a disease called IPEX syndrome where patients lack regulatory T cells, the investigators found no defect in Treg function in this animal model. Rather, autoimmunity was driven by activation of CD4+ T cell and B cell effectors by a particular cytokine called interferon gamma. This was surprising since a different family of interferon cytokines (Type 1 interferon), but not interferon gamma (Type 2 interferon), had previously been linked to the development of human autoimmunity.
The paper’s first author, Andrea Largent, is a former research scientist (now University of Washington graduate student) in the CIIT lab of corresponding author Dr. Shaun Jackson, principal investigator in the research institute and associate professor of pediatrics at the University of Washington School of Medicine. Other contributors include Dr. Eric Allenspach, CIIT principal investigator and assistant professor of pediatrics at the University of Washington School of Medicine; Dr. David Rawlings, CIIT director and professor of pediatrics at the University of Washington School of Medicine; and Dr. Jane Buckner, president of the Benaroya Research Institute, as well as other colleagues at both institutions.
“This research gives us more insight into how activating mutations in STAT1 cause human immune dysregulation, as well as helping us understand the role that STAT1 and different types of interferons may play in patients with other more common autoimmune disorders, such as lupus,” Jackson said.
He stressed the importance of studying patients with rare genetic disorders causing problems with the immune system — either vulnerability to infection or the development of autoimmunity — to learn how the human immune system functions.
“The most obvious link from our study to polygenic [caused by multiple genes] autoimmunity is to lupus,” Jackson said. “Our findings show how important Type II interferon (interferon gamma) might be in the development of lupus, whereas most in the field think that Type I interferon is the most important.
“Thus, beyond treating STAT1 GOF patients, this research points toward Type II interferon inhibitors as a potential therapeutic target, which could change how we treat patients with autoimmune disorders like lupus,” he said.
The study team next hopes to pinpoint the specific cell type(s) essential for inflammation in the mouse model, potentially leading to cell-specific therapies to eliminate or control the inflammatory cells in patients affected by this syndrome.
The research was supported by National Institutes of Health, as well as the Lupus Research Alliance, Seattle Children’s Research Institute, Children’s Guild Association Endowed Chair in Pediatric Immunology, Hansen Investigator in Pediatric Innovation Endowment, and the Benaroya Family Gift Fund.
— Colleen Steelquist